Lecture 15 hypoxia fetal and asphyxia of the newborn
The structure of perinatal mortality
Prematurity (50%).
Intrauterine hypoxia:
Stretching;
Hypoxia in childbirth.
Vices of development.
Infection.
Accident or injury not related to childbirth.
Other non-classified causes.
In absolute frequency, the most common cause of perinatal mortality is intrauterine asphyxia. The development of placental insufficiency and asphyxia of the fetus is associated with the complex of both maternal and fruit factors, including the adaptive possibilities of the fetus.
Factors affecting the oxygenation of the fetus
External environment:
Atmospheric oxygen pressure.
Maternal factors:
The concentration of hemoglobin and its affinity for oxygen;
Cardiovascular and respiratory adaptation of the mother.
Placental factors.
1. Physiological:
The rate of cord and uterine blood flow.
2. Structural:
The area of \u200b\u200bthe diffusion surface of the Epithelium Vorsin;
The thickness of the diffusion membrane of the Vorsin;
Diffusion shunts.
Fruit factors:
Concentration and predominate type of hemoglobin;
Cardiac emission and the distribution of blood flow.
Fruit adaptation mechanisms for hypoxia
High hemoglobin concentration.
High affinity of fetal hemoglobin (FHB) to oxygen.
High blood flow rate.
The rate of perfusion of the fetus organs is higher than the physiological need for oxygen.
Anaerobic glycoliz.
Classification of hypoxia fett
Chronic.
The aggravation of chronic.
Hypoxia classification
Hypoxic:
Hypoxia mother (extragenital pathology);
Placental failure (placenta detachment).
Gemic:
Fetal diseases with disorders of oxygen binding (hemolytic disease).
Circulatory:
Pupovina compression;
Congenital heart disease.
Tissue:
Incomplete utilization of oxygen with tissues in violation of enzymatic systems.
The main causes of hypoxia (distress) of the fetus
Placental insufficiency.
Pathology of the fetus.
Cord compression.
Hypoxia mother.
Placental insufficiency is characterized by a gradual decrease in the transmission of oxygen and nutrients to the fetus.
The passage of nutrients is the first function that is broken with FPN with the formation of a delay of intrauterine fetal growth, for the decrease in the respiratory function of the placenta with the formation of hypoxia. Persistent hypoxia causes anaerobic metabolism and optosis of the fetus. Thus, a significant clinical manifestation of chronic placental insufficiency is the delay in the growth of the fetus.
Under the SZRP of the fetus, the incomprehension of its sizes with normal for a given period of pregnancy is understood. The initial criterion for the presence of a SZRP in a child is to reduce the value of its body weight and (or) growth characteristic of gestational age, for 2 weeks (or more) less than the actual one.
By unifying the terminology in accordance with the ICD-10, we consider it expedient to denote the term "asymmetric form of SZRP" a small mass of the fetus for this gestational age (RO.5.0), the term "symmetric SZRP form" - a small fetal size for a given gestational age (RO.5.1 ), and the term "hypotrophy" - pathology associated with fetal failure (RO.5.2).
Etiology and Pathogenesis SZRP are reflected in Fig. 101.
Fig. 101.Etiology and Pathogenesis SZRP
When generalizing the causes of the development of the Fetal SZRP are reduced to the following.
1. Metabolic disorders due to various pregnancy complications.
2. Congenital anomalies or intrauterine infection.
3. Insufficiency of production of fetal growth hormones or pathology of their receptors.
The main directions in the treatment of insufficiency of the placenta function are as follows.
1. Normalization of uterine-placental blood circulation.
2. Normalization of the gas exchange between the organism of the mother and the fetus.
3. Improving the metabolic activity of the placenta.
4. Impact on the fetal body, which is a placenta (paraplventory exchange path).
Principles of placental insufficiency theory
Infusion therapy.
Anabolic, nootropic therapy (actovegin, carnitine chloride, Instenon, orotat potassium, riboxin, etc.).
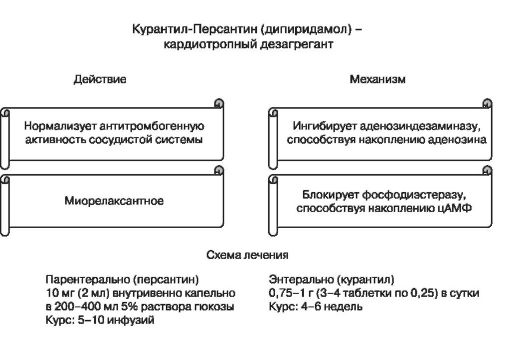
Degrementary therapy (kuraltyl, aspirin, low molecular weight heparins, pentoxifillain, xanthinol nicotine, etc.).
Antioxidant therapy (ascorbic acid, tocopherol).
Tocolytic therapy.
Ozone therapy.
Etiotropic therapy.
1. Anabolic therapy
Aktovegin- Hemoderivat low molecular weight peptides and nucleic acids.
Basic action- an increase in the energy metabolism of the cell. Action mechanisms.
Increases intracellular consumption and glucose transport five times.
Increases the disposal and consumption of oxygen.
Stimulates lipid biosynthesis.
Chloride carnitine
The main pharmacological effect- Increasing the energy exchange of the cell.
Action mechanisms.
Performs intracellular transport Acetyl Coenzyme - and in mitochondria β - Singing long chain fatty acids and pyruvate.
Increases acetylcholine products.
Stimulates the synthesis of protein and phospholipids of cell membranes.
Stimulates cholesterol synthesis.
Instenon- three-component nootropic drug.
This isfillin:
Reduces the total peripheral resistance of vessels;
Increases the minute volume of the heart.
Eatent:
It gives a nootropic effect, activating respiratory and vascular centers, a limbic system and a reticular formation.
Hexobendine:
Selectively stimulates intracellular metabolism, increasing the utilization of glucose and oxygen when the anaerobic glycolysis is activated under hypoxia.
2. Disaggregation and anticoagulant therapy
 Low molecular weight heparins.
Low molecular weight heparins.
Fractionrine (calcium pressure) 0.3 ml (7500 units) per day subcutaneously.
Kleksan (sodium enochaparin) 0.2 ml (20 mg) per day subcutaneously.
Multifacetic influence on the fetoplacentage complex has medical ozone. Local ozone effect: disinfecting activity against bacteria, viruses and mushrooms. System Effect: Improving the rheological properties of blood and microcirculation as a whole; activation of enzyme systems of antioxidant protection; stimulation of oxygen-dependent organism processes; Strengthening the activity of immunocompetent cells.
A fundamental impact on the perinatal exodue is the course of pregnancy and the functioning of the fetoplacentar complex, as well as the flow of birth and birth.
In the absence of the effect of conservative therapy, the operational delivery is shown - the cesarean section, and in the second period of birth, with the head in the cavity of the small pelvis - obstetric nippers, with a pelvic preview - the extraction of the fetus for the pelvic end.
Prevention of fetal hypoxia in childbirth
Termination of relatives.
Lateral position of the woman in labor.
Infusion therapy.
Inhalation of oxygen.
Tocolytic therapy.
Intrahamemic infusion.
To date, the main criterion for the state of the newborn is the assessment on the apgar scale, which determines not only the degree of hypoxia, but also (indirectly) the need for resuscitation measures (Table 22).
Note:6-7 points - mild hypoxia; 4-5 points - high-degree hypoxia; Less than 4 points - severe hypoxia.
The reasons for the asphyxes of newborns are reflected in Table. 23.
Procedure for resuscitation events
Heated (T \u003d 32-33 ° C).
Restoration of respiratory tract:
Suction of mucus;
Intubation and Sanation of trachea and bronchi.
Breath Support:
Bag Ambo;
Hardware IVL;
Naloxone.
Circulation support:
Infusion therapy;
Cadiotonics: Dopamine, Dobtreks.
The indirect heart massage is carried out with a stable bradycardia lasting more than 15-30 C and heart rate below 60 UD / min on
background of IVL.
Table 23.
The causes of asphyxia of newborns
Group of reasons | Etiological factors | Clinical manifestations |
Pup view puzzles pelvic preview Wrong positions Obstetrician tongs | Blood impairment Hypovolemia shock |
|
Medications | Narcotic analgesics sedatives | Foreignness of breathing |
Congenital pathology | Intrauterine infection | Cardiopulmonary failure |
Mother's disease and pregnancy complications | Sugar diabetes Eclampsia RH-conflict | Hyponcemia anemia Maconial aspiration |
Exogenous and yatrogenic | Childbirth in the cold pneumothorax, mediastines on the background of IVL | Hypothermia Heart and Lungs |
Infant mortality from PRD causes in: 45.9% of cases - congenital defects of the heart and blood circulation system; in 32.9% - multiple defects; in 18.4% - spina Bifida.and other vices of the nervous system. Thus, a substantial reserve of decline in infant mortality is to improve the organization and improving the quality of prenatal diagnosis.
Ways to reduce perinatal morbidity and mortality
Competent maintenance of the prenatal period.
Wide prenatal screening.
Training of specialists in the methods of prenatal diagnosis and interpretation of data.
Attracting the knowledge of the high perinatal risk of experienced specialists and consultants.
Expert assessment of perinatal mortality cases.
Staffing staffing staff.